By Dr. Lisa Hepworth, Class of 2012
Edited by Dr. Peg Miller, ADDL Pathologist
 Septic arthritis is a concern for equine practitioner every time intra-articular corticosteroids are administered, a puncture would is unnervingly close to a joint, a foal enters the hospital with omphalophlebitis and lameness, or an arthroscopy is performed to remove a carpal bone chip. What one must remember is that those joints may not all be septic, and if septic, bacteria may not be the only responsible organism. Healthy joints are vital to the performance of an equine athlete, and accurate assessment of the cause behind a “blown up” joint is essential to successful treatment.
Septic arthritis is a concern for equine practitioner every time intra-articular corticosteroids are administered, a puncture would is unnervingly close to a joint, a foal enters the hospital with omphalophlebitis and lameness, or an arthroscopy is performed to remove a carpal bone chip. What one must remember is that those joints may not all be septic, and if septic, bacteria may not be the only responsible organism. Healthy joints are vital to the performance of an equine athlete, and accurate assessment of the cause behind a “blown up” joint is essential to successful treatment.
The pathogenesis of synovitis and arthritis is diverse. The most common mechanisms include hematogenous bacterial or fungal infection, direct inoculation by a penetrating object such as a wire or twig, iatrogenic inoculation during intra-articular injection, aseptic reactions to intra-articular pharmaceuticals, and post-surgical infections. All of these can lead to bacterial arthritis, reactive arthritis, or fungal arthritis (Singer, E. R. 2008).
Bacterial infection is by far the most common cause of equine septic arthritis. Joint sepsis is suspected with total protein values above 4.0 g/dL, leukocyte counts >20,000/mL in adults and >10,000/mL in foals, and polymorphonuclear count >90% on cytologic examination. However, these changes are not specific for sepsis, and many may occur with reactive arthritis. In a study of equine septic arthritis by Schneider *1998), routes of infection were classified as intra-articular injection, penetrating wounds, post-surgical, idiopathic, and sepsis in foals. In that study, intra-articular injection was the most common cause of bacterial arthritis in adult horse; sepsis was the most common cause in foals.
In the study by Schneider, Streptococci were the responsible bacteria in most post intra-articular injection and post-surgical infections. For traumatic wounds and septic foals, the most common bacteria were Enterobacteriaceae, such as Escherichia coli, Proteus, Enterobacter, Klebsiella, Citrobacter, and Salmonella.
When a septic joint is non-responsive to aggressive antibiotic therapy, fungal causes should be considered. Immunosuppressed horses are at higher risk for fungal arthritis (Cohen, 2008). Cause of immunosuppression range from intra-articular steroid administration to pituitary pars intermedia dysfunction. Cohen (2008) reports 7 cases of fungal arthritis or osteomyelitis in adult horse and foals. Clinical presentation was similar to that with bacterial arthritis, but the condition progressed despite aggressive antibiotic treatment. Isolated fungal organisms included Aspergillis, Scedosporium, Candida albicans, Candida tropicalis, Candida parasilopsis, and Candida utilis. In the case of a Standardbred filly (Cohen), the affected joint contained fibrin exudate that adhered to the synovial membrane and articular cartilage and extended into the dorsal and palmar pouches. As the arthritis progressed, full-thickness cartilage defects developed with radiolucencies in subchondral bone. After months of aggressive treatment, the filly became pasture-sound with a poor prognosis for an athletic future, but potential for use as a brood mare.
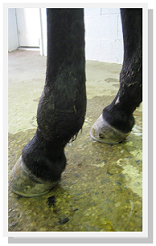
A case of Candida utilis was recently diagnosed at Purdue University. The horse was presented with septic arthritis following injection of corticosteroids, hyaluronic acid and amikacin into the tarso-crural joint. The recommended lavage and surgical treatment were initially declined by the owner. The course of therapy included antibiotic regional limb perfusions, intra-articular lavage and antimicrobials, and arthroscopy and arthrotomoy to remove fibrin and flush the joint. After Candida utilis was cultured from surgical samples of synovial fluid, synovial membrane and intra-articular fibrin, systemic and instar-articular treatment with fluconazole was initiated. The horse returned home with improvement, but re-presented with a grade 4/5 lameness shortly after the course of fluconazole was completed.
Upon re-presentation, subchondral bone cysts were noted radiographically in the distal aspect of the tibia and were suspected to communicate with the joint. Fluconazole treatment was re-instituted and interleikin-1 receptor protein antagonist therapy was initiated to reduce inflammation. Initially, the horse appeared to improve; however, the joint became more painful and at times the horse was non-weight bearing. The discomfort of the patient prompted a prognostic CT examination to determine the extent of osteomyelitis and articular cartilage damage. The CT revealed a pathologic fracture of the distal tibia and multiple articular cartilage defects that communicated with the subchondral bone. The owner elected humane euthanasia. The distal tibial fracture and articular defects of the tarso-crural joint were confirmed at necropsy. Fungal organisms were not detected postmortem by culture or histologic examination.
This case, along with the 7 previously reported cases of equine fungal arthritis emphasize the importance of not ruling out fungal causes in septic joints, especially those with intra-articular corticosteroid injection. Though rare, yeasts and fungi should always be considered in cases of septic arthritis that are non-responsive to aggressive antibiotic therapy. The prognosis for these patients is poor, and if a high-motion joint is involved, athletic soundness is unlikely even if the infection is resolved.
References
- Cohen, J.M., Ross, M.W. and Busschers, E. (2008) Diagnosis and management of Candida utilis infectious arthritis in a Standardbred filly. Equine vet. Educ. 20, 348-352.
- Madison, J.B., Reid, B.V. and Raskin, R.E. (1995) Amphotecerin B treatment of Candida arthritis in two horses. J. Am. Vet. Med. Ass. 206, 338-341.
- Reilly, L.K. and Palmer, J.E. (1994) Systemic candidiasis in four foals, J. Am. Vet. Med. Ass. 205, 464-446.
- Schneider, Robert K. (1998) Common bacteria encountered in septic arthritis. AAEP Proceedings.
- Sherman, K.M., Myhre, G.D. and Heymann, E.I. (2006) Fingal osteomyelitis of the axial border of the proximal sesamoid bones in a horse. J. Am. Vet. Med. Ass. 29, 1607-1611.
- Singer, E.R. (2008) Clinical challenges of persistent articular sepsis. AAEP Proceedings.