In August 2011, an epidemic arose in the European Nation. Cattle farms were suddenly experiencing high loss with limited signs of fever, anorexia, and decrease in milk production up to 50%.6 In three weeks, mortality rate ranged from 20 to 70%.7 The disease spread and began causing abortions, stillbirths, dystocia, and congenital abnormalities by the fall of 2011.6,7 In November, the etiologic agent was named the “Schmallenberg virus” by the Friedrich-Loeffler-Institut in a local German town.6 The virus is an Orthobunyavirus from the Bunyaviridae family; the enveloped, single-stranded RNA virus has been identified in over 2,100 ruminant (sheep, goat, cattle, and bison) farms in Europe.6,7,8 The susceptibility of wild ruminants or swine is currently unknown.6,7
The Schmallenberg virus closely resembles the Akabane, Aino, and Shamonda viruses in the Simbu serogroup of Orthobunyaviruses.6,7 It is unknown how the Simbu viruses first arose or where they originated, but they exist in African, Asian, Australian, and Middle Eastern countries.6,7 This virus family mainly causes mild clinical signs that can resolve within days; however, serious reproductive abnormalities can arise in infected pregnant females.6 The major mode of transmission for Orthobunyaviruses is through insect vectors such as mosquitoes and biting midges (Culicoides spp.).6,7 The midges are considered amplification vectors for the virus.7 Insect vectors for these viruses exist in North America; their potential to transmit the disease is under investigation.6 Transplacental transmission has also been documented in clinical cases between dam and offspring.6,7 Because of the high morbidity, spread of the disease must be monitored through live animals and germplasm, such as semen and embryos.6 Currently, there is no evidence that the virus can be transmitted through animal products such as meat or to humans.6 In research trials, the incubation period was 2 to 5 days after inoculation.7 A short viremic stage in cattle persisted for 6 days post-inoculation.7 Fetal infection cannot be detected until parturition or abortion.7
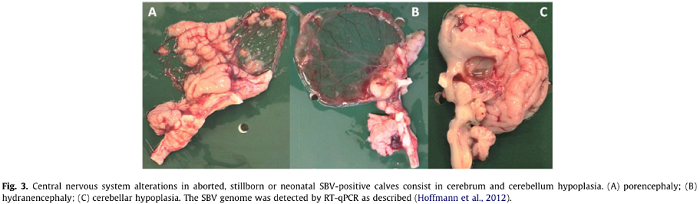
Clinical signs of Schmallenberg virus infection vary among animal populations. In adult ruminants, reduced milk production, hyperthermia, anorexia, watery diarrhea, lethargy, and increased incidence of abortions and congenital malformations can occur.2,6 Adult sheep, goats, and cattle are usually asymptomatic, or any mild clinical signs resolve within a week.7 Infected fetuses can be stillborn, premature, or mummified.1,2,7,9 The congenital malformations are those of the arthrogryposis hydranencephaly syndrome.7,9 Offspring at or near term can also have signs of ataxia, paralysis, muscle atrophy, joint malformations, behavioral abnormalities, abnormal vocalization, hyperexcitability, flaccid paralysis, inability to suckle, excessive lacrimation, and blindness.7,1 Malformation and clinical signs correlate to the stage of development at which the fetus was infected.7 These reproductive problems are more common in sheep and goats than in cattle farms.6 In one study, experimentally infected calves had fever, viremia, and diarrhea.7
The differential diagnosis includes infectious, genetic, toxic, or nutritional conditions that cause abortions, congenital malformations, or systemic illness.7 Recognized causes of these conditions include bovine viral diarrhea virus, pestiviruses of small ruminants, bovine herpesvirus type 1, foot-and-mouth disease virus, bluetongue virus, bovine ephemeral fever virus, Veratrum californicum toxicosis, Lupinus spp. toxicosis, gestational protein or mineral deficiency, and spider lamb syndrome.7,8
Serum or EDTA-preserved whole blood is the preferred sample for virus identification in adult animals.7 Optimally, samples should be collected during acute disease.7 For diagnosis in case of abortion, chilled or frozen samples of brain, spleen, and blood should be submitted to a diagnostic laboratory.7,8 Current diagnostic testing in the European Union nations is focused on real-time reverse transcriptase polymerase chain reaction (RT-PCR) for the Schmallenberg virus in all suspected cases.6,7 Commercial PCR kits are available for use in local establishments.8 Confirmatory testing includes indirect immunofluorescence and virus neutralization assay.7 Mass testing can be conducted through a newly developed enzyme linked immunosorbent assay (ELISA).6,7
Sample submission8
- Live Animals
- EDTA Blood
- Serum (≥2 mL cooled)
- Stillborn or Affected Neonates
- Virus Detection
- Cerebrum & Brainstem
- Amniotic fluid
- Placenta
- Meconium
- Antibody Detection
- Pericardial fluid
- Blood (preferably pre-colostral)
- Histopathology
- Fixed central nervous system tissues & spinal cord
Gross lesions at necropsy in bovine fetuses or neonates include hydranencephaly and porencephaly, hypoplasia of the central nervous system, micromyelia, dilated cystic cerebellum, musculoskeletal abnormalities, and subcutaneous edema.4,8,9 Characteristic musculoskeletal abnormalities include jaw, vertebral, and limb deformities such as brachygnathia inferior, ill-formed lower mandible, torticollis, scoliosis, kyphosis, or arthrogryposis.2,9 Unilateral spinal muscle atrophy may be concurrent.2 Virus isolation is successful from cerebrum, cerebellum, brain stem, medulla oblongata, and spinal cord.4,9 Histologic evaluation can document encephalitis with lymphohistiocytic perivascular cuffing.4,9
Although research is underway, there is currently no effective vaccine for herd protection from the Schmallenberg virus.6 Preventive action to limit disease spread across Europe is focused on vector control.6
Case Example (January 2012, Belgium): A female Belgian Blue calf was born with hypertonia and hyperreflexia.3 The calf could not stand, had changing mentation, bilateral blindness, and ventrolateral strabismus. Absent conscious proprioception was apparent when placing the calf on its feet. At necropsy, the cerebral hemispheres had been replaced by two thin, fluid-filled cysts, consistent with severe hydrancephaly. The Schmallenberg virus was subsequently isolated from CNS samples.3
Viral spread depends on the natural history, environmental temperatures, and number or distribution of vectors and ruminant hosts.7 Although the virus has not been detected in the United States, action has been taken by the USDA Animal Plant Health Inspection Service to minimize risks of introduction of the Schmallenberg virus.6 There is currently a ban on import of European Union live ruminants to the United States due to the risk of bovine spongiform encephalopathy transmission.5,6 In addition, recent restrictions have been placed on the importation of bovine germplasm (semen and embryos) from the European union and countries that follow the EU legislation.5 Germplasm donors must test negative for the virus and be held in a vector-proof facility for 30 days prior to and during collection processes.5 This restriction is placed on any embryo or semen from bovine, ovine, and caprine sources since June 1st, 2011.6 If the shipments include products collected before June 1st, appropriate statements on the official export health certificate must confirm the validity of the date.5 Cervid and camelid germplasm, ruminant products, and ruminant by-products are not currently restricted for importation.5
In the United States, a passive surveillance plan for Schmallenberg virus has been instituted under the Animal Plant Health Inspection Services in collaboration with veterinary diagnostic laboratories.6 Animals submitted to diagnostic laboratories with signs or lesions consistent with Schmallenberg virus infection will be analyzed for the virus.1 The National Veterinary Services Laboratory (NVSL) has acquired the rRT-PCR from the Friedrich-Loeffler-Institut in Germany for diagnostic purposes.1 The NVSL is developing its own virus neutralization serologic assay.7 In America, additional surveillance attention should be placed on wild cervids, bison, and feral swine populations.7 Although the virus is not currently present in the United States, quick detection can help avoid disease establishment if it should appear in our country.6 If you suspect Schmallenberg virus in a herd, please contact your State animal health official or the APHIS Veterinary Services Area Veterinarian-in-Charge immediately.7
References
- Anonymous. “Schmallenberg Virus Guidance for U.S. Veterinary Diagnostic Laboratories.” March 2012. pdf
- Garigliany, M-M, et al. “Schmallenberg virus: A new Shamonda/Sathuperi-like virus on the rise in Europe.” Antiviral Research; 95 (2012) 82-87. (Pictures)
- Garigliany, M-M, et al. “Schmallenberg Virus in Calf Born at Term with Porencephaly, Belgium.” Emerging Infectious Diseases Letters; 18:6 (2012) 1005-1006.
- Hahn, K, et al. “Schmallenberg Virus in Central Nervous System of Ruminants.” Emerging Infectious Diseases Letters; 19:1 (2013) 154-155.
- USDA APHIS Animal Health. “Schmallenberg Virus Information.” March 2012. www.aphis.usda.gov/animal_health/animal_diseases/schmallenberg/index.shtml
- USDA Veterinary Services. “European Orthobunyavirus; or ‘Schmallenberg’ Virus.” March 2012 APHIS Factsheet.pdf.
- USDA Veterinary Services. “Schmallenberg Virus: Case Definition & Guidance.” APHIS. March 2012.pdf.
- World Organization for Animal Health. “Schmallenberg Virus.” OIE Technical Factsheet.May 2012.pdf
- Herder V, Wohlsein P, Peters M, Hansmann F, Baumgärtner W. Salient lesions in domestic ruminants infected with the emerging so-called Schmallenberg virus in Germany. Vet Pathol 2012; OnlineFirst, published on May 18, 2012 as doi:10.1177/0300985812447831