By Dr. Bill Wigle, ADDL Pathologist
Since the liver has extensive functional reserve, relatively severe injury must be present before specific clinical signs appear. In early stages of hepatobiliary disease, clinical signs are nonspecific and include anorexia, vomiting, diarrhea, weight loss, PU/PD and dehydration. In advanced disease, specific signs include jaundice, bleeding tendencies, hepatomegaly or microhepatica, hypoglycemia, hepatic encephalopathy, gastrointestinal ulceration, ascites and superficial necrolytic dermatitis.
Conditions affecting the gastrointestinal tract, endocrine, urinary, nervous, cardiovascular and hematopoietic systems, as well as neoplasia and systemic infections, can result in the same nonspecific signs seen with early hepatobiliary disease. Such non-hepatic disorders have secondary effects on the liver (reactive hepatopathies) resulting in increased serum liver enzymes which then require differentiation from primary liver disease. In fact, the majority of instances where liver enzyme levels are increased do not represent primary hepatic disease.
A complete blood count, serum chemistry panel, and urinalysis form the primary screening tests for liver disease. Hematologic tests are primarily used to determine if a systemic disease process is present and to determine if jaundice is pre-hepatic in the presence of anemia.
Alanine transferase (ALT) and aspartate transferase (AST) are “leakage” enzymes which become elevated when hepatocytes are damaged. These enzymes have both a short half-life and, if serum high levels persist with repeated measurements, ongoing disease is suggested. ALT is more specific for hepatic disease than is AST.
Alkaline phosphatase (ALKP) and gamma-glutamyl transpeptidase (GGT) are “cholestatic” or “inducible” enzymes. Bile stasis causes increased production of these enzymes which are located in the cell membranes of bile canaliculi (ALKP) and bile duct epithelium (GGT). These enzymes may also be induced by drugs or corticosteroids. Increases in ALKP alone have been associated with hepatic neoplasia and benign hepatic nodular hyperplasia. The bone isoform of ALKP may also be increased in young dogs prior to closure of growth plates or adult dogs with osteogenic tumors.
Once the presence of primary liver disease is established, the diagnostic process should proceed in a sequential manner. Elevated liver enzymes can reflect damage or the presence of inflammation in the liver, but they provide no estimate of hepatic functional capacity. Routine chemistry panel values that are indicative of liver function include bilirubin, blood glucose, cholesterol, albumen and blood urea nitrogen. Generally, advanced hepatic disease is present when these values become abnormal.
Bilirubin becomes elevated when there is excessive hemolysis, hepatocellular dysfunction and cholestasis or obstruction of the extrahepatic bile ducts. Blood glucose is reduced after loss of more than 70% of hepatic function and is often low in animals with portosystemic shunts. Cholesterol levels in serum increase in cases of extrahepatic biliary obstruction and are decreased in cases of portosystemic shunts. Reduced serum albumin is observed due to decreased synthesis in hepatic failure when about 75% of liver function is lost. Blood urea nitrogen (BUN) is reduced as a result of the liver’s inability to convert ammonia to urea. This finding is most commonly associated with portosystemic shunts.
Plasma ammonia has been shown to be a sensitive and specific indicator for the presence of congenital portosystemic shunts as well as for acquired shunts. The volatility of ammonia requires that blood be collected in an EDTA-coated tube and that the specimens be placed on ice with NH3 measurement being performed within 30 minutes. This test is essentially limited to specialty practices or those with access to a properly equipped local laboratory since samples cannot be shipped for testing.
A coagulation profile may be useful if hepatic biopsy is planned. Dogs with chronic hepatitis, with or without cirrhosis, have been shown to have reduced coagulation factors due to impaired hepatic synthesis.
Measurement of serum bile acids are more sensitive as a function test and become elevated sooner in the course of hepatic disease than the above biochemical parameters. This test is most appropriate when animals have persistent elevated hepatic enzymes and are not jaundiced.
Urinalysis demonstrating bilirubinuria in cats suggests either hepatobiliary disease or hemolysis. The presence of ammonium biurate crystals in dogs and cats occurs with portosystemic shunts.
 The above laboratory findings are useful in establishing the presence of hepatobiliary disease, but do not define it well. Liver biopsy provides the means to classify the type of disease, plan for specific treatment and has prognostic value. Liver biopsy specimens may be obtained via fine-needle aspiration, blind percutaneous or ultrasound-guided needle biopsy, laparoscopy and exploratory laparotomy. Diffuse liver disease may be successfully diagnosed by fine-needle aspiration or blind percutaneous biopsy. Ultrasound-guided needle biopsy, laparoscopy and laparotomy are more diagnostic when lesions are focal. Standardized histologic criteria for diagnosis of liver disease in small animals have recently been published to aid in applying biopsy findings to clinical decision making.
The above laboratory findings are useful in establishing the presence of hepatobiliary disease, but do not define it well. Liver biopsy provides the means to classify the type of disease, plan for specific treatment and has prognostic value. Liver biopsy specimens may be obtained via fine-needle aspiration, blind percutaneous or ultrasound-guided needle biopsy, laparoscopy and exploratory laparotomy. Diffuse liver disease may be successfully diagnosed by fine-needle aspiration or blind percutaneous biopsy. Ultrasound-guided needle biopsy, laparoscopy and laparotomy are more diagnostic when lesions are focal. Standardized histologic criteria for diagnosis of liver disease in small animals have recently been published to aid in applying biopsy findings to clinical decision making.
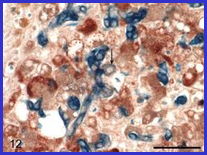
Hepatic biopsy is also the means of obtaining specimens for quantitative copper analysis to diagnose copper associated hepatopathy. A 1-2 gram specimen is required for chemical analysis. Levels above 1000 ppm are diagnostic. Obtaining a liver biopsy also provides a specimen for virus isolation or culture for bacteria and fungus.
A combination of diagnostic modalities is required to confirm and define hepatocellular disease in small animals. Early detection and intervention is required to maximize the effectiveness of specific therapy.
Suggested Reading:
- Bexfield N: 2006. Diagnosis of canine liver disease. In Practice 28:444-453.
- Rothuizen J and Twedt DC: 2009. Liver biopsy techniques. Vet Clin N Amer Sm Anim 39:469-480
- Watson PJ: 2004. Chronic hepatitis in dogs: a current understanding of the aetiology, progression, and treatment. Vet J 167:228-241.
- WSAVA LIVER STANDARDIZATION GROUP: 2006. Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. Elsevier, Toronto, Canada